The Biomedical Engineering (BME) department at Armour College of Engineering hosted the presentation of capstone design projects at the end of the spring 2015 semester. The event was well attended by BME faculty, fellow students, affiliated clinical mentors, judges and friends of BME.
Six teams of Armour College undergraduate students presented the medical devices they designed and built for their senior design course. The Bio-EARN team earned the top spot at the competition. The yearlong course consists of two semester-long courses: BME 419: Introduction to Design Concepts in Biomedical Engineering and BME 420: Design Concepts in Biomedical Engineering. Both classes are supported by a grant through the National Institutes of Health (NIH). Jennifer Kang-Mieler and Derek Kamper, both Associate Professors of Biomedical Engineering, advise the students. The students also have expert mentors in the field to offer feedback and advice on their projects.
The course functions like a design firm where students are encouraged to immerse themselves in a problem, build prototypes for testing, and then refine their designs. Students assemble their own teams and interact with their medical mentors throughout the year. By the end of the academic year, each team is to have designed and built a working prototype.
Beyond the classroom the students enter their projects in contests across the country. This year, LMNT Biotech submitted their project to the American Society for Artificial Internal Organs (ASAIO) Student Design Contest. Each team submitted their projects to the NIH sponsored DEBUT competition which will announce winners on August 24, 2015.
Each team designed and built a prototype device to solve a unique problem.
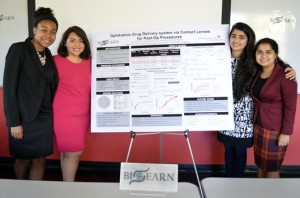
Bio-EARN
Team: Edna Arias (BME, 5th year), Aparna Singh (BME, 5th year), and Roshani Patil (BME, 5th year) Nicole Patterson (BME, 5th year)
Clinical Mentors: William Mieler, M.D., Director of Ocular Oncology, Director of Residency and Vitreoretinal Fellowship Training, Professor of Ophthalmology – Retina Service, Cless Family Professor in Ophthalmology, Vice Chair for Education at University of Illinois College of Medicine at Chicago; and Jennifer Kang-Mieler, Ph.D.
Millions of people undergo eye surgeries each year in the United States alone. Although the risk of developing infection or inflammation after surgery is low, many patients fail to follow through with the 10-day eye drop treatment post-surgery. This can put these patients at risk for further damage to the eye or loss of vision. The Bio-EARN team focused on solving this problem by developing a hydrogel contact lens, VISELUTE, that allows for the controlled and sustained release of antibiotics for two weeks after a surgery. This method of treatment allows for a controlled and sustained delivery of the drug and promotes patient compliance.
Bioinnovate
Team: Emilija Jakimovska (BME, 4th year), Veronica Torres (BME, 4th year), Ian Thomas (BME, 5th year), and Nathan McMahon (BME, 4th year)
Clinical Mentors: Mike Ujiki, M.D. – NorthShore University Health System and Alex Deravianko, surgical research scientist – NorthShore University Health System
Many patients die each year while undergoing surgeries. If a surgery being performed is rare, the risk of complications or death can be very high. It is important that surgeons practice to ensure they are at the top of their game. Current surgical simulators do not provide adequate training for surgeons because they lack realistic tissue, there is no tactile feedback, and they aren’t accurate representations of the human body. These simulators are also expensive to purchase and maintain. Splenectomies are considered rare surgeries and the Bioinnovate team sought to create Precision4D, an artificial spleen to be used in an inexpensive, whole-body surgical simulator. The device mimics the consistency of human spleen, is cauterizable, has integrated vasculature, and functional blood flow to provide a realistic simulator experience.
Handstetics
Team: Danielle Albom (BME, 4th year), Yewande Taiwo (BME, 4th year), Mark Brezai (BME, 4th year), and Tracy Pfeffer (BME, 4th year)
Clinical Mentor: Derek Kamper, Ph.D.
Losing movement of the hands can be debilitating for people who have suffered a stroke. When a person is able to regain movement in their hands it can improve the quality of their life immensely. The Handstetics team sought to help people regain hand movement by developing FlexiForce, a glove that captures and tracks the movements of the hand during therapy and interfaces with a virtual reality game. Traditional forms of physical therapy can be unsuccessful due to lack of interest from the patient. The virtual game will provide patients with a fun and interactive way to do therapy that will keep them engaged. The glove will measure the movement of individual fingers and wrist and report it to a physical therapist who can use it to gauge the progress being made by the patient. The team’s device will be more cost effective and portable than similar devices, opening it up to be used by more people.
LMNT Biotech
Team: Ziyao Jiang (BME, 4th year), Medha Parulekar (BME, 5th year), Nicholas Welsh (BME, 5th year), and Tamara Gedankien (BME, 4th year)
Clinical Mentor: Mike Ujiki, M.D. – NorthShore University Health System and Alex Deravianko, surgical research scientist – NorthShore University Health System
Pancreatic adenocarcinoma accounts for the majority of all diagnosed pancreatic cancers and is very aggressive. The most effective treatment for this type of cancer is to surgically remove the tumors from the pancreas. This procedure is extremely challenging due to the consistency of the pancreatic tissue as well as its intricate location at the bottom of the abdominal cavity. Surgeons currently practice this procedure using virtual simulators that lack tactile feedback or cadavers and animal models that possess different mechanical properties than a living human pancreas. The LMNT Biotech team has been working to develop PANCREATiX, a pancreatic surgical simulator that mimics a living human pancreas’ consistency and vascular network. The team’s design is also cauterizable and has realistic tumors incorporated to make the simulated organ as realistic as possible.
Medical Innovation Solutions (MI Solutions)
Team: Ameer Ghouse (BME, 4th year), Chaudhry Ahmad (BME, 4th year), Jose Rios (BME, 5th year), and James de la Cruz (BME, 5th year)
Clinical Mentor: Kenneth Tichauer, Ph.D.; Derek Kamper, Ph.D.; and Jennifer Kang-Mieler, Ph.D.
Birth asphyxia can be damaging to a newborn child’s brain or even fatal and happens when reduced cerebral blood flow causes a reduction in oxygen in the brain. The Medical Innovation Solutions team focused on developing the MI-15 device to monitor oxygen consumption levels in the brain of newborns and to act as an early warning system to prevent birth asphyxia. Current methods to monitor oxygen consumption are invasive, can involve radiation (using MRIs), and are time consuming. The team’s device uses the principles of pulse oximetry to estimate oxygen consumption by calculating the difference of oxygen in arterial and venous blood. The team’s solution allows for quick and continuous monitoring of oxygen consumption.
Turbo5000
Team: Precious Eboh (BME, 4th year), Mehal Shah (BME, 4th year), Mateo Garcia (BME, 5th year), and Jia-Hui Shi (BME, 4th year)
Clinical Mentors: Derek Kamper, Ph.D.; Jennifer Kang-Mieler, Ph.D.; and Laura Miller, PhD, CP; research scientist/prosthetist – Rehabilitation Institute of Chicago, clinical associate professor – Department of Physical Medicine and Rehabilitation at Northwestern University
In developing countries there are many people living with above the knee amputations. In these countries there is a lack of trained prosthetists and it can be difficult for many people to travel long distances to a prosthetic shop. If they do have the ability to get to a shop, the labor intensive process of creating a custom socket using plaster casting can take up to a month. Many prosthetic devices used by these people are donated from other countries. This means that most prosthetics do not have sockets that are custom fitted to the user. Many people end up not using the device because of the pain, rashes, and swelling that can occur from ill fitting prosthetics. The Turbo5000 team sought to solve these problems by creating Rapid Socket, a portable imaging system that can be taken to remote locations in developing countries. The device they developed quickly generates a 3D scan of person’s residual limb from a set of 2D images. Their design consists of a rotating drum that houses a camera. The drum rotates and takes an image every six degrees. These images are then used to generate a 3D model of the person’s residual limb which will then be used to mold a custom socket for a prosthetic device.